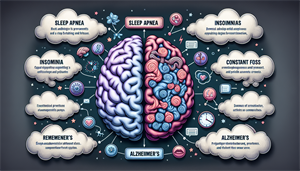
Understanding the Connection Between Sleep Apnea and Alzheimer's
Have you ever wondered why a good night’s sleep is so crucial? Poor sleep can affect more than just your mood and energy levels. It can have serious implications for your cognitive health. What’s even more concerning is that chronic sleep disorders, like sleep apnea and Alzheimer’s, may contribute to cognitive decline – a connection often overlooked. Understanding and addressing these conditions can significantly improve health outcomes, highlighting the importance of sound sleep and its role in maintaining brain health.
Key Takeaways
Sleep apnea, characterized by sleep interruptions and reduced oxygen to the brain, is linked to cognitive decline and Alzheimer’s disease through mechanisms such as sleep fragmentation and intermittent hypoxia. Common risk factors for both sleep apnea and Alzheimer’s include age, gender, obesity, smoking, sedative/alcohol use, and family history, with diagnostic challenges for Alzheimer’s patients due to overlapping symptoms and pathological complexities. Treatment options for sleep apnea, such as CPAP therapy, alternative treatments like BiPAP and Auto CPAP, lifestyle changes, and preventive measures, may improve cognitive health and potentially slow Alzheimer’s progression.
The Sleep Apnea-Alzheimer's Connection
Sleep Apnea, a prevalent sleep disorder, involves continual episodes of shallow or paused breathing during sleep, which results in sleep interruptions and insufficient oxygen supply to the brain. This chronic condition, including central sleep apnea, has been associated with a myriad of health complications, such as heart disease, stroke, and cognitive decline. The connection between sleep apnea and cognitive decline, particularly Alzheimer’s disease, has garnered significant attention in recent years. Sleep disordered breathing, such as sleep apnea, can have a profound impact on overall health and well-being.
Two main mechanisms through which sleep apnea exacerbates cognitive decline and Alzheimer’s disease are sleep fragmentation and intermittent hypoxia. Sleep fragmentation refers to frequent awakenings or shifts between stages of sleep, leading to poor sleep quality. On the other hand, intermittent hypoxia refers to episodes of significantly reduced or completely paused airflow during sleep, causing a drop in blood oxygen levels. Both of these processes have serious implications for brain health and function.
These processes, which are fundamental to severe obstructive sleep apnea, have been implicated in generating neurodegenerative changes associated with Alzheimer’s disease. Sleep deprivation is associated with increased levels of beta-amyloid and tau proteins in the brain, which are related to the development of Alzheimer’s disease. Thus, understanding and managing sleep apnea is not just about improving sleep quality but also about mitigating risks for cognitive decline and Alzheimer’s disease.
Sleep Fragmentation
Often seen in severe sleep apnea, sleep fragmentation involves recurrent awakenings or transitions to lighter sleep stages, disrupting the deep sleep that is essential for proper rest. This disruption in sleep patterns can result in elevated levels of Alzheimer’s-related proteins in the brain, leading to adverse effects on memory and cognitive function in obstructive sleep apnea patients.
As a consequence of sleep fragmentation, there is a rise in the levels of two Alzheimer’s-related proteins: amyloid and amyloid-beta. Individuals suffering from sleep fragmentation may present signs and symptoms such as: increased objective sleepiness, decreased psychomotor performance, degraded mood, loud disruptive snoring, witnessed apneas during sleep, excessive daytime sleepiness, waking up feeling tired, headaches upon waking, dry or sore throat, and trouble with concentration. Therefore, tackling sleep fragmentation is crucial in managing sleep apnea and its associated risks.