Can You Develop Sleep Apnea After Surgery?
If you’re wondering, “can you develop sleep apnea after surgery?” the short answer is yes. Surgery can influence sleep patterns and potentially lead to sleep apnea due to anesthesia, sedation, and stress on the body. In this article, we’ll explore how surgical procedures might trigger or worsen this condition, and what that means for your postoperative care and recovery.
Key Takeaways
Surgical procedures, anesthesia, and sedation can exacerbate or even trigger obstructive sleep apnea (OSAS) by causing alterations in sleep patterns and increasing the likelihood of airway collapse, potentially leading to various complications. Identifying sleep apnea in surgical patients is critical for managing and minimizing perioperative complications, which can be achieved using screening tools like the Berlin, ASA, and STOP-BANG questionnaires, as well as methods like nocturnal pulse oximetry. Proper perioperative management of sleep apnea, including preoperative evaluation, attentive intraoperative care, and rigorous postoperative monitoring, is essential to reduce the risk of complications and improve patient outcomes.
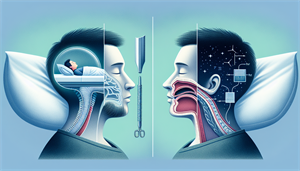
Surgery's Impact on Sleep Apnea Development
Surgery, a routine part of our healthcare landscape, can have an unexpected yet significant impact on the development of obstructive sleep apnea syndrome (OSAS). The connection between the two may not seem apparent initially, but it becomes clearer when we delve into the effects of anesthesia, sedation, and surgical stress on our sleep patterns and breathing. As a result, sleep medicine plays a crucial role in understanding and managing this connection.
Intermittent and recurrent episodes of partial or complete obstruction of the upper airway during sleep are the main features of obstructive sleep apnea, causing breathing pauses and disturbances in sleep patterns. This condition, often referred to as unrecognized obstructive sleep apnea, can lead to symptoms such as: daytime fatigue, loud snoring, morning headaches, difficulty concentrating, irritability, and increased risk of high blood pressure, heart disease, and stroke. Its association with surgical procedures becomes more significant when you consider factors such as anesthesia and surgical stress.
It’s not just about the surgery itself; it’s also about the after-effects. Postoperative complications are a major concern, and an increase in their likelihood is a risk we cannot afford to ignore. Alterations in sleep patterns, such as an initial drop in sleep efficiency, REM sleep, and slow-wave sleep, may occur after surgery. Although these changes are typically temporary, they can potentially exacerbate or even trigger sleep apnea. This is because after surgery, the Apnea-Hypopnea Index, a measure of sleep apnea severity, tends to rise, indicating a potential worsening of the condition.
Anesthesia and Sedation Effects
As fundamental elements of most surgical procedures, anesthesia and sedation can significantly influence sleep apnea. They can exacerbate the condition by increasing the likelihood of airway collapse, which, in turn, can lead to postoperative cardiovascular complications. It’s not just the immediate effects during surgery; the impact extends well into the postoperative period, affecting ventilatory responses and even the arousal response in patients with sleep apnea.
The arousal response, the body’s mechanism to awaken us from sleep in response to threats such as airway obstruction, plays a critical role in sleep apnea patients. Anesthesia, however, can inhibit this response, increasing the risk of prolonged episodes of apnea during sleep. The effects of anesthesia and sedation on sleep apnea are not isolated; they are part of a broader impact that surgery can have on sleep patterns. Surgical stress, for instance, can lead to disruptions in sleep patterns and a reduction in