How Diabetes and Sleep Apnea Affect Each Other
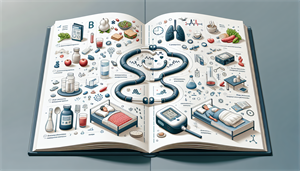
It’s essential to uncover how these conditions can escalate in tandem, complicating treatment and management. In the following sections, we’ll dissect the relationship between diabetes and sleep apnea, shed light on their combined prevalence, and provide a guide to recognizing symptoms, navigating treatments, and implementing monitoring practices to keep them both in check.
Key Takeaways
-
There is a bidirectional relationship between diabetes and obstructive sleep apnea (OSA), with each condition potentially worsening the other. Shared risk factors include obesity and insulin resistance, with OSA contributing to impaired glucose metabolism and diabetes potentially exacerbating OSA.
-
Diabetic patients have a higher prevalence of sleep apnea than the general population, with rates varying significantly, particularly in obese diabetic patients.
-
These findings support the need for regular screening for sleep apnea in diabetic individuals. Effective management of sleep apnea in diabetic patients involves CPAP therapy, weight management, and lifestyle changes such as diet and exercise. These interventions can improve both sleep quality and blood sugar control, thereby addressing both conditions simultaneously.
The Bidirectional Relationship Between Diabetes and Sleep Apnea
A bidirectional link exists between diabetes and obstructive sleep apnea (OSA), with each condition potentially exacerbating the other. Obesity and insulin resistance are shared risk factors of note.
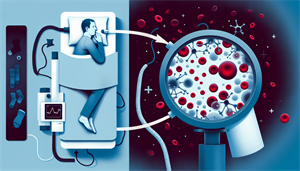
People with OSA often experience an increase in blood sugar levels impacting insulin release and thus affecting glucose levels throughout the day. Sleep apnea disrupts glucose metabolism in individuals with type 2 diabetes, which can contribute to glucose intolerance. This impaired glucose metabolism occurs through sympathetic activation, oxidative stress, inflammation, and neuroendocrine dysregulation.
The disruption is further aggravated by intermittent hypoxia, a consequence of sleep apnea, which directly affects hepatocytes leading to elevated cellular glycogen content and increased gluconeogenic enzymatic activity.
How Sleep Apnea Contributes to Insulin Resistance
Two key mechanisms - intermittent hypoxemia and sleep fragmentation - can cause sleep apnea to lead to insulin resistance, a precursor to diabetes. These disruptions to normal sleep patterns interfere with glucose metabolism, raising the chances of developing type 2 diabetes, especially in untreated obstructive sleep apnea cases.
Hypoxemia, a condition marked by low levels of oxygen in the blood, affects insulin effectiveness by impeding the distribution of insulin to cells, reducing cell responsiveness to insulin, and causing elevated blood glucose levels, leading to impaired glucose tolerance. Intermittent hypoxemia, in particular, alters glucose metabolism by reducing glucose-induced insulin secretion and inducing a metabolic shift from aerobic to anaerobic processes.
On the other hand, sleep fragmentation, particularly in instances of obstructive sleep apnea, leads to deteriorated glucose tolerance and decreased insulin sensitivity, thereby contributing to insulin resistance. Continuous positive airway pressure (CPAP) therapy, a common treatment option for sleep apnea, can effectively mitigate these issues.
How Diabetes Can Lead to Sleep Apnea
Despite the complex and not fully understood relationship between diabetes and sleep apnea, there is evidence to suggest that diabetes may impact central respiratory control and potentially contribute to obstructive sleep apnea. This is due to: The influence of diabetic neuropathy on central regulation of respiration.